HIPAA was introduced to improve patient privacy and offer a basic guideline for medical professionals and insurance organisations while handling patient health information (PHI). Over the years, the Department of Health and Human Services (HHS) has updated the HIPAA Rules of Security and Privacy multiple times, the most recent being in March 2025, to ensure that the Act stays relevant to the evolving privacy breach risks and cyber attack threats.
This guide has been developed for medical health professionals or IT professionals in healthcare and insurance to offer a comprehensive understanding of HIPAA compliance that is essential to protect patient privacy and avoid legal risks.
In this guide, you’ll find:
The Need for HIPAA in 2025: Why Healthcare Cannot Afford to Take a Chance Anymore
As technology advances, more and more business entities and organizations handling PHI are falling prey to cyberattacks. According to the HIPAA Journal, in March 2025 alone, “1,754,097 individuals had their protected health information exposed, stolen, or impermissibly disclosed in healthcare data breaches.”
It’s a shocking number, but part of an alarming trend. Both January and February 2025 saw more than 2,000,000 patients impacted by HIPAA-related data breaches. These breaches not only put patients at risk of identity theft and other dangers, they also impede access to care by limiting clinic operations during recovery.
Data breaches can be very costly for healthcare organizations. In 2023, the average data breach cost in US healthcare was recorded to be $10.93M (IBM 2023 report).
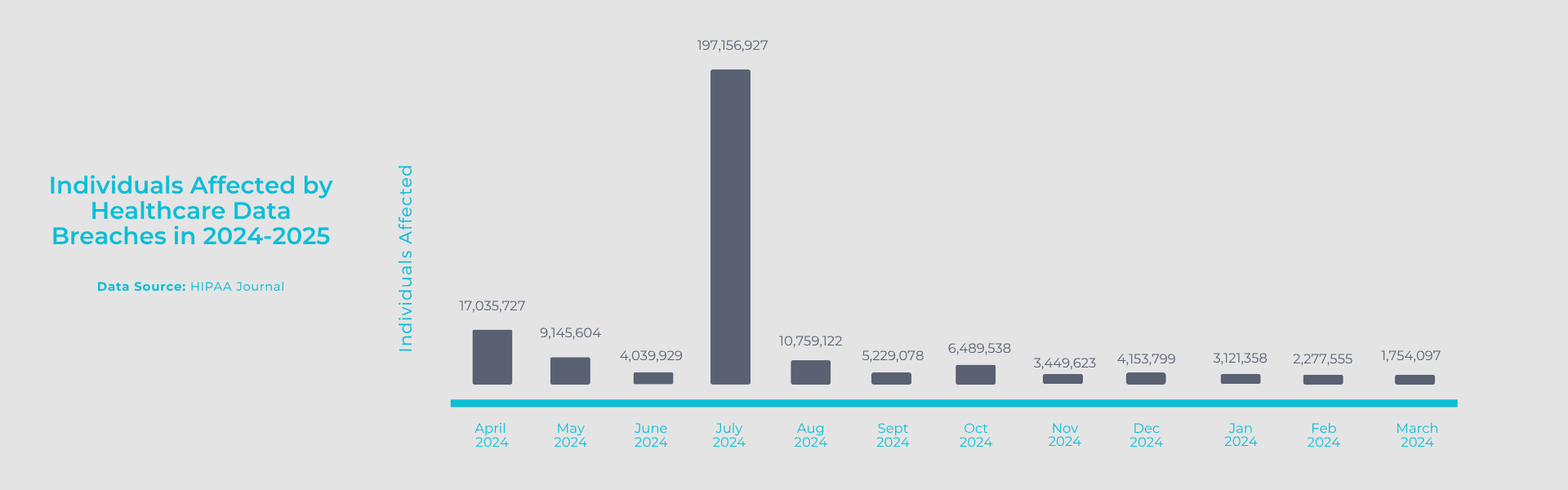
Source: HIPAA Journal
These numbers underline the need for stronger data protection tools and protocols to be established and maintained across healthcare organizations. HIPAA compliance training is the first step towards ensuring the privacy of health information, securing digital patient files and improving insurance portability.
What are the Main HIPAA Compliance Rules?
There are 7 different types of HIPAA rules; the most important among them are the HIPAA Privacy Rules and the HIPAA Security Rules. According to the HHS, HIPAA rules apply mainly to two categories – covered entities and business associates. All healthcare organizations, clinics, medical professionals and pharmacies fall under covered entities. Business associates refer to the non-medical organizations, businesses, and service providers who help healthcare organizations carry out their activities. Now, let’s understand the different HIPAA rules.
HIPAA Privacy Rule
The HIPAA Privacy Rule deals with the protection of medical records and patient health information. By law, the HIPAA Privacy Rule applies only to covered entities. However, in cases where healthcare organizations and clinics use the services of business associates to fulfil their activities, the Privacy Rule allows them to disclose PHI to the business associates on condition that they submit satisfactory assurances on their use and management of PHI. Healthcare organizations must offer HIPAA Compliance Training to their employees so that they understand how to handle patient information responsibly and be aware of patient rights.
HIPAA Security Rule
The HIPAA Security Rule covers all policies and protocols related to creating, storing, handling and deleting electronic protected health information or ePHI. This rule applies to both covered entities as well as business entities and provides guidelines for implementing administrative, physical, and technical safeguards to protect patient information. The HIPAA Security Rule builds the foundation for developing strategies to prevent cyberattacks and data breaches.
HIPAA Breach Notification Rule
The HIPAA Breach Notification Rule defines the conditions under which covered entities must report data breach incidents to the affected individuals, the HSS, and in some cases the media. This rule also gives healthcare organizations a guideline on how to respond in the event of a data breach. Timely and transparent breach reporting is critical not just for regulatory compliance, but also for damage control, patient reassurance, and maintaining the credibility of a healthcare brand.
HIPAA Enforcement Rule
The HIPAA Enforcement Rule deals with the entire process of investigations, penalties, and hearings related to HIPAA violations and HIPAA breach penalties. Applicable to both covered entities and business associates, the rule is enforced by the Office for Civil Rights (OCR) and helps reinforce a culture of compliance. According to the HIPAA Enforcement Rule, the HSS can impose a HIPAA breach penalty of up to $50,000 per violation, depending on severity and intent of non-compliance.
HIPAA Transaction and Code Sets Rule
The HIPAA Transaction and Code Sets Rule establishes strict standards and formats for the electronic exchange of healthcare-related data, such as billing, insurance eligibility, and claims processing. The rule instructs healthcare organizations and business associates who transmit information electronically to use standard medical codes, and eliminate the use of duplicative and local codes. With the help of HIPAA Compliance Training courses, all healthcare organizations must familiarize their administrative staff about this HIPAA rule and ensure that their clinics comply.
HIPAA Identifier Standards Rule
The HIPAA Identifier Standards Rule requires the use of unique identifiers for healthcare providers (NPI – National Provider Identifier), health plans, and employers to streamline administrative processes and ensure accurate identification. This rule applies to all entities that interact with HIPAA-covered transactions.
HIPAA Omnibus Rule
The HIPAA Omnibus Rule was introduced in 2013 to strengthen HIPAA compliance and extend accountability of patient data protection to all organizations handling PHI, and not just the healthcare providers. It clarifies patients’ rights, enhances privacy protections, and tightens requirements for handling PHI. Understanding the Omnibus Rule is vital because it closes previous loopholes and holds organizations accountable across the entire data handling ecosystem – from cloud vendors to transcription services.
What are the latest HIPAA Updates from March 2025
The most recent HIPAA Update from March 2025 seek to improve security of medical systems and patient information. From mandating Multi-factor Authorizations (MFAs) and enhanced data encryptions to enforcing annual security audits, these updated regulations aim to close the long-standing security gaps across the board. Some of these are veru critical for healthcare organizations and clinics. Let’s look at the key takeaways from the March update.
1. Mandatory Multi-Factor Authentication (MFA):
Clinics must now implement MFA for all systems with patient data, adding extra protection against password-based breaches. From internal communications platforms, email accounts for communicating with patients, and CRMs, the regulation needs to be implemented across all digital tools and platforms used by healthcare organizations.
2. Enhanced Data Encryption Protocols:
Healthcare providers must use communication solutions that provide enhanced encryption both in transit and in rest. This move is aimed at reducing the risk of data leaks and encouraging the use of secure mail solutions that provide protection and confidentiality.
3. Annual Audits and Vulnerability Scanning:
Healthcare providers must now perform FULL security audits every year, reinforcing a culture of proactive data protection. Healthcare providers also need to onboard or consult security and privacy experts to run a complete security health scan of their systems and processes to identify gaps and fix them.
HIPAA Penalties, Fines and Legal Consequences
The cost of HIPAA non-compliance can be very heavy for healthcare organizations. First, you have the HIPAA Breach penalties from the ORC. But it doesn’t end there. HIPAA breaches have been shown to negatively impact care quality and access to care for months or even years afterwards. Clinics that suffer a large breach typically lose about 70% of patients within the first 6 months.
Take the Hospital Sisters Health System (HSHS) breach incident of 2023. The network of hospitals and clinics in Illinois and Wisconsin suffered a major data breach that exposed PHI of nearly 900,000 patients. As a result, HSHS is now facing at least four class action lawsuits, including allegations of negligence, misuse of tracking technologies, and employment privacy violations. Though HIPAA doesn’t permit private lawsuits directly, the plaintiffs are using HIPAA standards as the legal benchmark to prove the organization failed in its duty of care.
The threat of a data breach is very real, if not increasing. According to the HIPAA Journal, 734 large data breaches have been reported to the OCR in 2024.
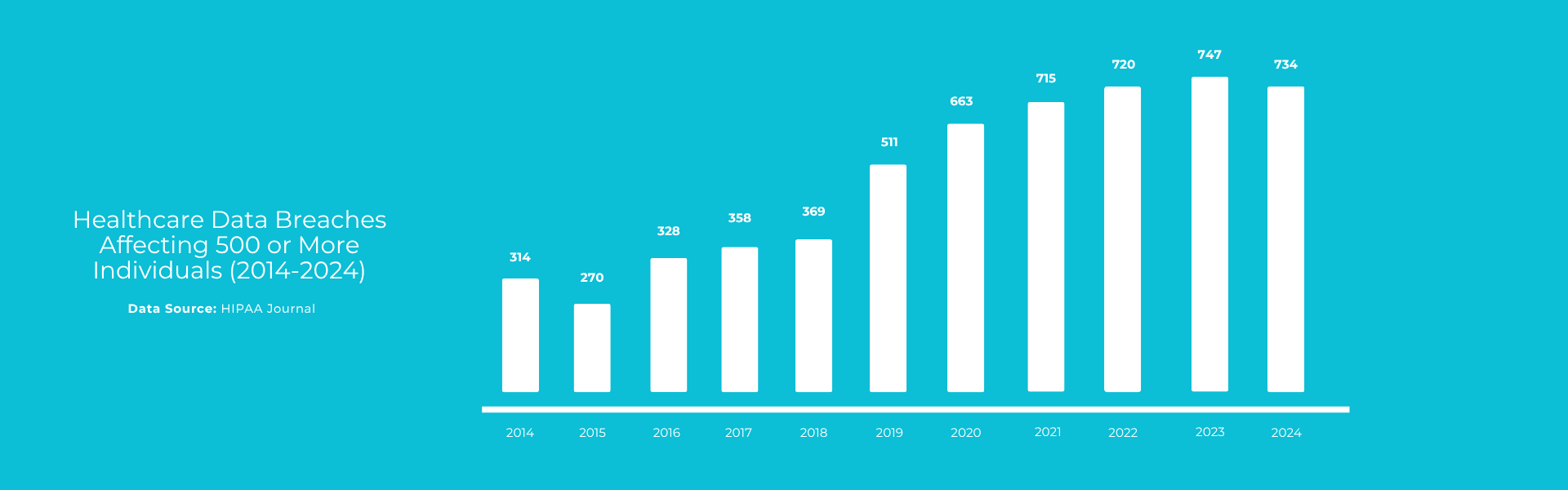
Data Source: HIPAA Journal
The most commonly cited reasons for levying HIPAA penalties include failure to assess risk, lack of proper HIPAA compliance training for staff, and delayed breach notifications. Hence, a proper understanding of HIPAA Compliance rules and reporting procedures is absolutely essential for all clinics and healthcare providers if they want to avoid penalties.
HIPAA penalties are broadly classified into civil and criminal. The HSS and the ORC is responsible for enforcing the penalty structure based on the level of negligence and the harm caused by the violation.
HIPAA Compliance Training for Healthcare Staff
In order to stay compliant with the HIPAA framework, healthcare organizations need to ensure that all their employees and their business associates follow the same rules and regulations. It’s a shared responsibility across every level of the organisation, from the front desk to the back office. The best way to ensure that all your employees are aware of their legal responsibilities, data handling protocols, and the consequences of non-compliance is to conduct a HIPAA Compliance Training course for them.
What Should HIPAA Training Cover?
HIPAA trainings are most effective when they are based on real-world healthcare settings and challenges. It should help you distinguish between data that is part of PHI and that which is not. It should also cover the entire gamut of patient rights when it comes to their medical health data and how to handle patient requests.
Effective HIPAA training will help your employees to identify, report and respond to potential security incidents and will equip them with the tools and platforms required to avert such risks.
Here’s what you need to remember when seeking HIPAA Compliance Training programs:
- Choose real-time or micro-modules with short interactive sessions for maximum retention and engagement.
- Ask for incident-based training if you’ve had a near-miss or a small breach.
- Opt for annual refresher courses so that you and the team can stay updated on the latest policy revisions and additions.
- It is always best practice to conduct a HIPAA compliance training course when onboarding a new employee.
Brightsquid’s HIPAA Privacy Compliance Training
To help healthcare teams stay compliant with ease and confidence, Brightsquid offers tailored HIPAA Privacy Compliance Training. Designed for busy medical professionals, our program includes interactive modules, real-life scenarios, compliance checklists, and progress tracking to ensure your staff not only understands HIPAA but also knows how to apply it.