
The year 2025 was not exactly the best for healthcare data security, but neither was it the worst. While over 57 million individuals were known to have been affected by healthcare data breaches last year, the industry sighed a little knowing that it was still an improvement over 2024 when the data of half the population of America was exposed in a single breach.. But are we calling it progress? Not yet!
Looking back at the biggest breaches and cyber incidents of 2025, a clear pattern emerges. Whether the organization was a healthcare provider, a government contractor, or a vendor handling sensitive data, the failures almost always involved third-party access, insecure communication channels, delayed detection, or gaps in training.
In this article, we review the top 5 healthcare data breach incidents of 2025, try to understand what went wrong, risk signals, and how you can be better prepared in 2026 and stay HIPAA compliant.
Top Five Healthcare Data Breaches in 2025
Breach disclosures throughout 2025 made one thing clear: healthcare cybersecurity is not stabilizing. In fact, it is evolving into a more dangerous and coordinated game. The attackers now seem to be staying away from attention-seeking big data thefts to more strategic and deliberate moves targeting smaller healthcare organizations. Here are the top 5 data breaches of 2025.
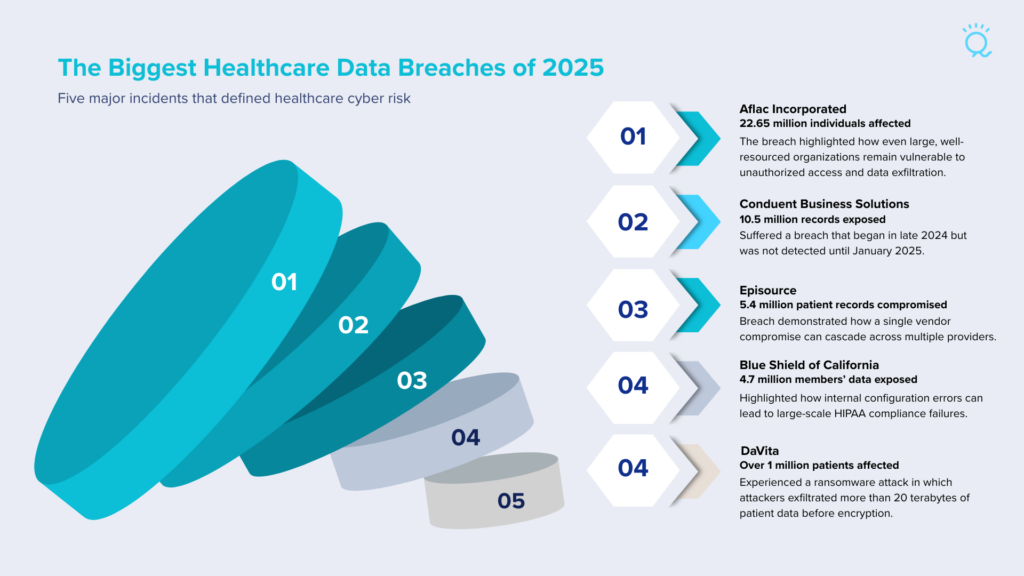
Aflac Incorporated Cybersecurity Incident – 22.65 million individuals affected
One of the biggest data breach incidents of 2025 started in June when insurance giant Aflac confirmed that hackers stole the personal and health information of roughly 22.65 million individuals. According to reports, the compromised information includes:
- Customer names and dates of birth
- Home addresses and government-issued ID numbers (passports, state IDs)
- Social Security numbers
- Driver’s license numbers
- Medical information and health insurance data
Conduent Data Breach – 10.5 million records exposed
Conduent Business Solutions, a large service provider supporting healthcare and government clients, suffered a breach that exposed the personal information of over 10.5 million individuals. The breach began with unauthorized access in October 2024 but wasn’t detected until January 2025. Public disclosure and notifications were delayed by several months, prompting multiple class-action lawsuits.
Episource Data Breach – Over 5 million patient records compromised
Episource, a healthcare technology and analytics provider, disclosed that attackers accessed and copied sensitive data from its systems affecting approximately 5.4 million individuals across more than 100 healthcare organizations. The data is said to have included
- Medical records
- Diagnoses
- Test results
- Insurance information
- Personal identifiers such as names and Social Security numbers
Episource’s breach demonstrates the risk of third-party vendors that hold large volumes of data for multiple insurers and providers. When one vendor is compromised, the impact cascades across many organizations and patients.
Blue Shield of California Exposure – Data of 4.7 million members shared
Blue Shield of California accidentally exposed sensitive member health data to Google and its advertising platform because of a misconfigured analytics tool. What is alarming is the fact that the misconfiguration persisted from April 2021 through January 2024 and was discovered only in February 2025.
This incident highlights that compliance risk isn’t always driven by hackers – it can arise from internal tool misconfigurations. Organizations must audit security configurations, including embedded analytics scripts and integrations to ensure PHI isn’t unintentionally shared.
DaVita Ransomware Attack – Over 1 million patients’ data
Dialysis provider DaVita disclosed that a ransomware group (Interlock) exfiltrated over 20 terabytes of data, affecting more than 1 million patients. The attack was detected in April 2025, but forensic analysis revealed that unauthorized access began in March. Compromised data has included demographic and clinical information, and portions of the stolen dataset have been leaked.
What These Top Five Incidents Tell Us About Healthcare Risk in 2025
- Third-party and vendor exposure continues to dominate. Breaches at Conduent and Episource show that one compromised vendor can impact millions of patients across multiple healthcare entities.
TAKEAWAY: Ensure you have a signed Business Associate Agreement with all vendors and review proof of their HIPAA compliance measures.
- Misconfigurations are a hidden threat. Blue Shield’s analytics error underscores that even non-malicious internal mistakes can result in massive PHI exposure.
TAKEAWAY: Have your IT configurations audited by IT security professionals.
- Detection delays are costly. Conduent’s timeline shows how long dwell times allow attackers to access deep data before discovery, increasing harm.
TAKEAWAY: Set up network monitoring that will detect suspicious or unauthorized activity within your IT environment.
- Data exfiltration is often more damaging than encryption. DaVita was not just encrypted, data was copied, illustrating that modern ransomware is as much about theft as disruption.
TAKEAWAY: Gone are the days when you could rely on your data backups to address ransomware attacks after the fact. Prevention has to be the priority.
- Incident response and transparency matter. Aflac’s rapid response and support services contrast with slower notification timelines that have drawn legal scrutiny in other breaches.
TAKEAWAY: Be prepared with an incident response plan.
Healthcare Data Outlook for 2026
Looking ahead, security leaders agree that these trends are likely to intensify in 2026 rather than fade. Attackers continue to move beyond straightforward encryption-based ransomware toward disruption-first attacks designed to interfere directly with healthcare operations with the additional threat of data leaks.
Instead of locking systems and negotiating quickly, newer attacks aim to corrupt or delete backups and even damage infrastructure, thereby extending recovery timelines and increasing pressure to pay by affecting care delivery. These incidents often resemble traditional ransomware events on the surface, but their true objective is to create maximum urgency through downtime and operational chaos.
Leadership attention must extend beyond technical safeguards to include workforce HIPAA training, cyberthreat awareness, secure communication infrastructure, vendor risk governance, and incident communication planning. Organizations that fail to address these areas face increased operational, regulatory, and reputational risk.
FAQ: Understanding the Healthcare Breach Outlook
- Why do healthcare breaches now cause more disruption even when fewer are reported? – Although the incidents may look like traditional ransomware attacks on the surface, a deep dive reveals breach patterns where attackers are prioritizing depth over scale. Instead of launching many attacks, they invest time in gaining trusted access through vendors or stolen login credentials. This allows them to remain undetected longer and cause more damage once discovered, including extended downtime and operational interference.
- Why are communication systems such a major risk area for healthcare operations – Most sensitive data moves through email, messaging, and file-sharing platforms. Even when systems are technically secure, improper use – such as misdirected messages or insecure sharing – creates openings attackers can exploit. Communication tools are often trusted by default, which makes them attractive targets.